Awards
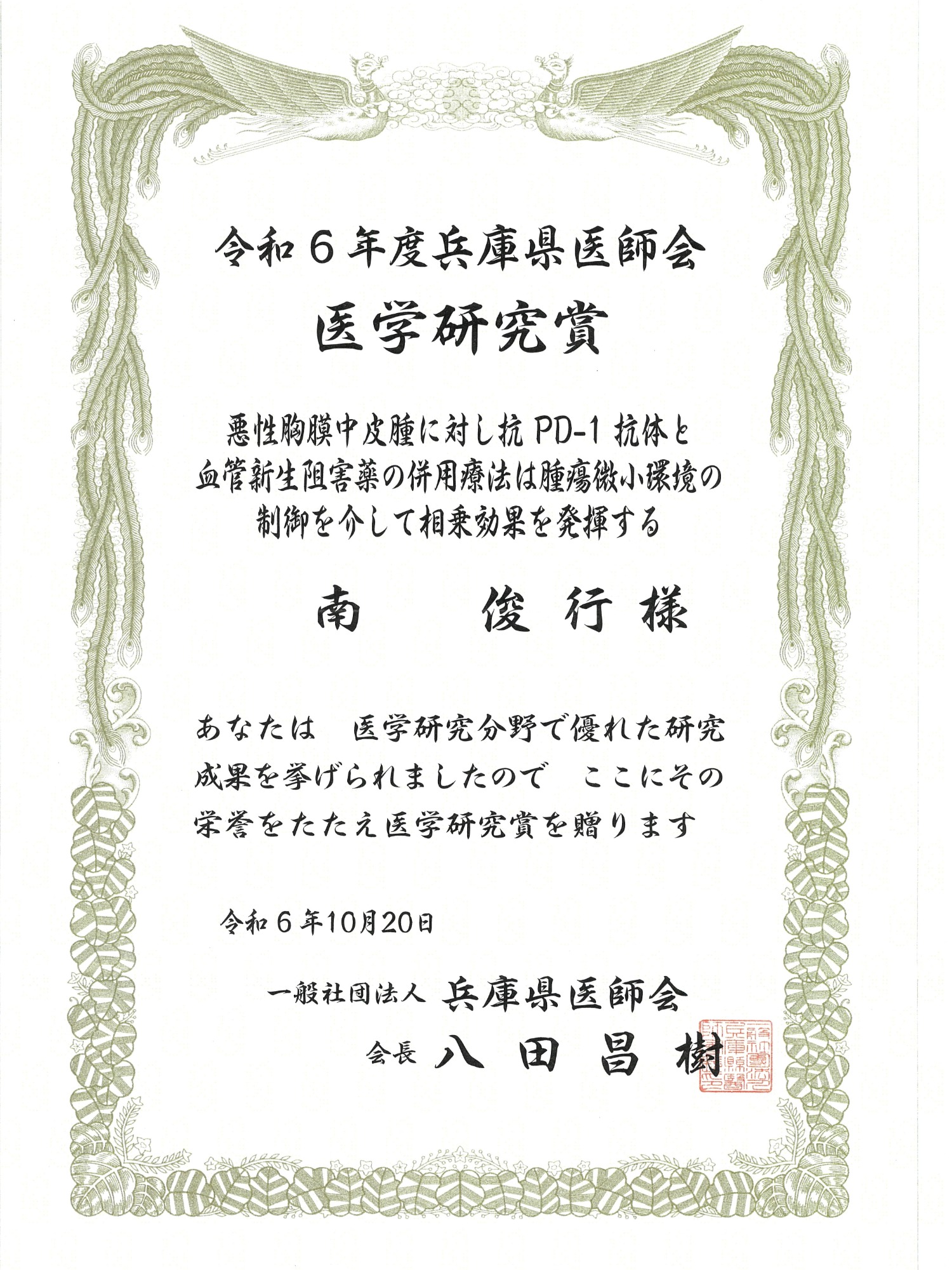
Received the 2024 Hyogo Prefectural Medical Association Medical Research Award (Minami Toshiyuki, Associate Professor, Department of Respiratory Medicine and Hematology)
Associate Professor Toshiyuki Minami of the Department of Respiratory Medicine and Hematology has been awarded the Hyogo Prefectural Medical Association Medical Research Award for FY2024. This award is given to those who have achieved outstanding research results in the field of medical research.
Name of the awarding organization
Hyogo Prefectural Medical Association
Research topic
Combination therapy of anti-PD-1 antibody and angiogenesis inhibitor exerts synergistic effects by controlling the tumor microenvironment in malignant pleural mesothelioma
Research Overview
Pleural mesothelioma (PM) is an asbestos-related, intractable malignant disease with a poor prognosis. In recent years, cancer immunotherapy using immune checkpoint inhibitors (ICIs), primarily anti-programmed cell death (PD)-1 antibodies, has brought about a new breakthrough in PM treatment. To maximize its antitumor effect, we evaluated whether the angiogenesis inhibitor nintedanib could enhance the antitumor effect of anti-PD-1 antibodies. Although nintedanib failed to suppress mesothelioma cell proliferation in vitro, it significantly suppressed mesothelioma cell growth in a mouse subcutaneous transplant model. Furthermore, combination therapy with anti-PD-1 antibodies and nintedanib induced significant necrosis in mesothelioma subcutaneous tumors and dramatically suppressed tumor growth compared with nintedanib monotherapy. The mechanism of this synergistic effect was not the activation of cytotoxic T cells as initially assumed, but the result of quantitative and qualitative suppression of tumor-associated macrophages (TAMs). Based on these results, combination therapy of anti-PD-1 antibody and nintedanib may be a new treatment option for PM patients.
Research Background
For PM, cisplatin + pemetrexed combination therapy was established as the standard treatment in 2003, but no new treatments have been established for a long time since then. Among them, the effectiveness of the anti-PD-1 antibody nivolumab was shown in 2019, and the combination therapy of nivolumab and the anti-cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) antibody ipilimumab in 2021 was shown, and they can now be used in clinical practice, clearly improving the prognosis of PM patients. However, unlike non-small cell lung cancer, for PM, biomarkers that predict the effectiveness of ICI have not been identified, and at present, the only scientifically-based treatment is ICI and platinum drug + pemetrexed combination therapy, so treatment options are uncertain and extremely limited. Therefore, the establishment of new, more effective treatments is an urgent issue for PM patients.
In PM, angiogenesis is said to be correlated with prognosis, and the angiogenesis inhibitor bevacizumab has been confirmed to have an additional effect on cisplatin + pemetrexed therapy and is covered by insurance in some countries. It has also been suggested that angiogenesis inhibitors may enhance the effects of cancer immunotherapy. Therefore, we decided to investigate the combination therapy of anti-PD-1 antibodies and angiogenesis inhibitors as translational research that can be applied to clinical practice.
Research methods and results
When we investigated the expression of angiogenic factors in human mesothelioma cells, we found that the cells produced multiple types of angiogenic factors and their receptors. Therefore, we conducted preclinical studies using nintedanib, a multi-kinase inhibitor that is already used in clinical practice for idiopathic pulmonary fibrosis, as an angiogenesis inhibitor. Nintedanib did not suppress mesothelioma cell proliferation in vitro, but it significantly suppressed tumor growth in a mouse subcutaneous tumor model. Furthermore, combination therapy with anti-PD-1 antibody and nintedanib induced significant necrosis in mesothelioma subcutaneous tumors and dramatically suppressed tumor growth compared to nintedanib monotherapy. The mechanism of this synergistic effect was not the antitumor effect mediated by cytotoxic T cells as initially assumed, but rather that nintedanib suppresses the production of chemokines derived from mesothelioma cells, quantitatively reduces tumor-associated macrophages (TAMs), and promotes the nuclear translocation of NF-kB through dephosphorylation of Smads, thereby changing the phenotype from tumor-promoting M2 type to antitumor M1 type. On the other hand, nintedanib induces the expression of PD-1 in TAMs and PD-ligand 1 (PD-L1) in tumors, and the establishment of the PD-1/PD-L1 signal inhibits the phagocytic ability of TAMs. It is expected that the phagocytic ability of TAMs can be restored by combining anti-PD-1 antibodies, and combination therapy with nintedanib and anti-PD-1 antibodies is considered to be a reasonable treatment strategy that complements each other's weaknesses.
Source of research funds etc.
Japan Society for the Promotion of Science Grant-in-Aid for Scientific Research 18K15962, 20K08555
Hyogo Medical University Medicine Research Activation Grant 2020
Nippon Boehringer Ingelheim Research Grant
Publication
Lung Cancer. 2023 Jun:180:107219.