Achievements
A medical paper published in the journal "Hypertension" reveals that "nocturnal hypertension" in diabetic patients is a risk factor for worsening diastolic function even before the onset of heart failure
A paper summarizing the results of a joint study by Dr. Kimiichi Kiwawara, Lecturer Manabu Kadotani, and Professor Hidenori Koyama of the Department of Department of Diabetes Endocrinology and Clinical Immunology, Associate Professor Masataka Igeta, Professor Takashi Daimon, Professor Masaki Asakura, and Professor Masaharu Ishihara of the Department of Cardiovascular and Renal Dialysis Medicine, was published in the journal Hypertension, published by the American Heart Association (AHA). (Hypertension. 2024;81:172–182. DOI:10.1161/HYPERTENSIONAHA.123.21304.)
Please see below for details of the research.
Topic
Nocturnal Hypertension and Left Ventricular Diastolic Dysfunction in Patients With Diabetes With the Absence of Heart Failure: Prospective Cohort HSCAA Study
Author of the paper
Yonekazu Kidawara, Manabu Kadoya, Masataka Igeta, Akiko Morimoto, Akio Miyoshi, Miki Kakutani-Hatayama, Akinori Kanzaki, Kosuke Konishi, Yoshiki Kusunoki, Takashi Daimon, Masanori Asakura, Masaharu Ishihara and Hidenori Koyama
Research Summary
In recent years, heart failure caused by reduced left ventricular diastolic function has been increasing, and its pathology and risk factors are attracting attention. It has long been pointed out that diabetes is related to this heart failure, and unstable blood glucose fluctuations have been thought to be one of the causes. However, the effect of "nocturnal hypertension" on left ventricular diastolic function in diabetic patients is unknown, and no research has been reported to date that directly compares the effect of nocturnal hypertension on left ventricular diastolic function in diabetic patients with that of non-diabetic patients before the onset of heart failure.
In this prospective study, our research group revealed for the first time that non-dipper and riser types of "nocturnal hypertension" in diabetic patients can predict the progression of diastolic dysfunction independently of patient backgrounds at the stage before heart failure develops. The results of this study demonstrated the risk of "nocturnal hypertension" in diabetic patients at a stage before heart failure develops, and have provided important knowledge for future heart failure prevention strategies that can be applied to clinical practice.
*This research is the result of collaborative research with Associate Professor Igeta Masataka, Professor Daimon Takashi, Department of Medical Statistics, Professor Asakura Masaki, Department of Cardiovascular and Renal Dialysis Medicine, and Chief Professor Ishihara Masaharu.
Research Background
In Japan, the incidence of heart failure has been increasing in recent years, and attention has been focused on the pathology of heart failure with preserved ejection fraction (HFpEF), in which the systolic function of the left ventricle is preserved but the diastolic function is impaired, and prevention and identification of risk factors are urgent issues. Diabetes has long been identified as a risk factor for this type of heart failure, and unstable blood glucose fluctuations have been suggested as a possible cause. On the other hand, diabetic patients frequently suffer from "nocturnal hypertension," which is assumed to affect left ventricular diastolic function, but no studies have been reported that directly compare diabetic patients with non-diabetic patients and prospectively examine the impact of HFpEF on the development of heart failure.
Research Methods and Results
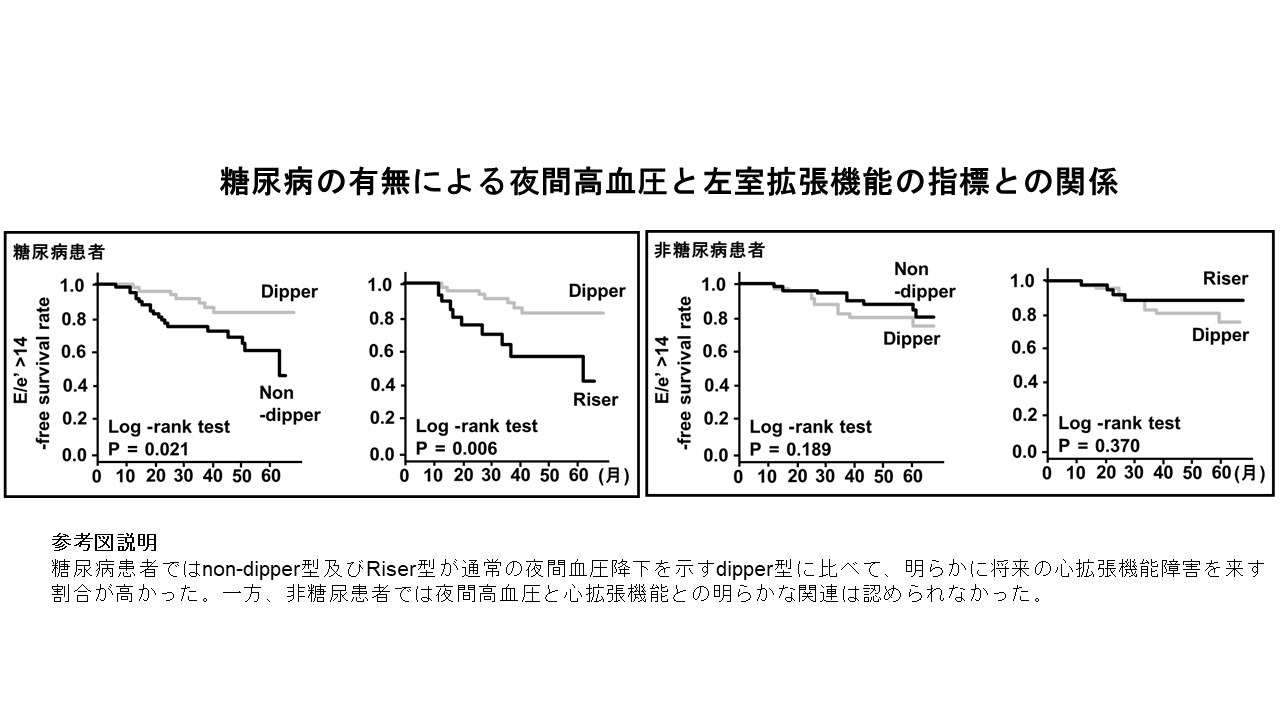
As part of the previous HIC project, we are conducting the Hyogo Sleep Cario-Autonomic Atherosclerosis (HSCAA) cohort study at our university to clarify how objectively quantified sleep, autonomic nervous function, and nocturnal blood pressure fluctuations are involved in the onset of various metabolic diseases, arteriosclerosis, and cardiac and renal dysfunction. In this study, we prospectively examined how nocturnal hypertension (non-dipper type, riser type) is related to the progression of cardiac diastolic dysfunction in 154 diabetic patients and 268 non-diabetic patients who had not yet developed heart failure among patients enrolled in the HSCAA cohort study.
Kaplan-Meier analysis showed that non-dipper and riser types of diabetic patients were significantly more likely to develop future diastolic dysfunction than dipper types who showed normal nocturnal blood pressure drops. On the other hand, no clear association between nocturnal hypertension and diastolic function was observed in non-diabetic patients. In a Cox proportional hazards model that examined the effects of these factors, including patient background, non-dipper and riser types in diabetic patients still showed a significant association with a decline in diastolic function in the future. Furthermore, in an analysis using a linear mixed model, the riser type, especially in diabetic patients, was significantly associated with the rate of change in diastolic function for each observation year.
The results of this study confirmed that "nocturnal hypertension" is an important predictor of the progression of cardiac diastolic dysfunction in diabetic patients, even before the onset of heart failure. This indicates that in order to prevent the future onset of heart failure, it is necessary to pay particular attention to the presence of "nocturnal hypertension" in diabetic patients, in addition to blood glucose fluctuations, and we believe that this has provided extremely important knowledge for the clinical setting in which heart failure is treated.
Future challenges
This study showed that "nocturnal hypertension" in diabetic patients is a risk factor for worsening cardiac diastolic function. In the future, it will be necessary to examine whether blood pressure treatment intervention for diabetic patients with "nocturnal hypertension" can actually contribute to preventing a decline in cardiac diastolic function. In addition, basic research is also needed to understand the mechanism by which "nocturnal hypertension" in diabetic patients affects the decline in cardiac diastolic function and what effect it has on the substance of left ventricular myocardial cells.
Source of research funds etc.
Grants-in-Aid for Scientific Research: JP19K19421 (Kadotani Manabu), JP20K18944 (Morimoto Akiko), JP18K17399 (Kadotani Miki), JP19K19446 (Kosaka Yoshie), JP18K08531 (Koyama Hidenori)
FY2018-2021 HIC project research funds (Hidenori Koyama)