About the Corporation
Multidisciplinary collaboration results in the publication of a paper on postoperative subcutaneous emphysema following laparoscopic surgery
A research group led by Kazuma Ito, a hospital assistant in the Department of Gastroenterological Surgery Division of Lower Gastrointestinal Surgery Hyogo Medical University College School of Medicine (located in Nishinomiya, Hyogo Prefecture; President: Keiichiro Suzuki), and others (supervised by Lecturer Kozo Kataoka and Chief Professor Masataka Ikeda), collaborated with a variety of professionals, including nurses and radiologists, to investigate the occurrence of subcutaneous emphysema, a complication of laparoscopic surgery, and its relationship to patient background and surgical factors, based on data from approximately 2,500 patients, and explored the incidence rate and risk factors.
In this study, regular palpation by nurses during surgery and thorough postoperative X-ray examinations were performed, which allowed for a more accurate indication of the incidence rate. In addition, by promptly communicating the results of palpation to doctors and coordinating with them, the risk was minimized, and the incidence rate of severe subcutaneous emphysema was lower than in previous reports.
This is the largest report on subcutaneous emphysema to date, and the publication of this paper was made possible through the cooperation of a wide range of professionals, including doctors and nurses.
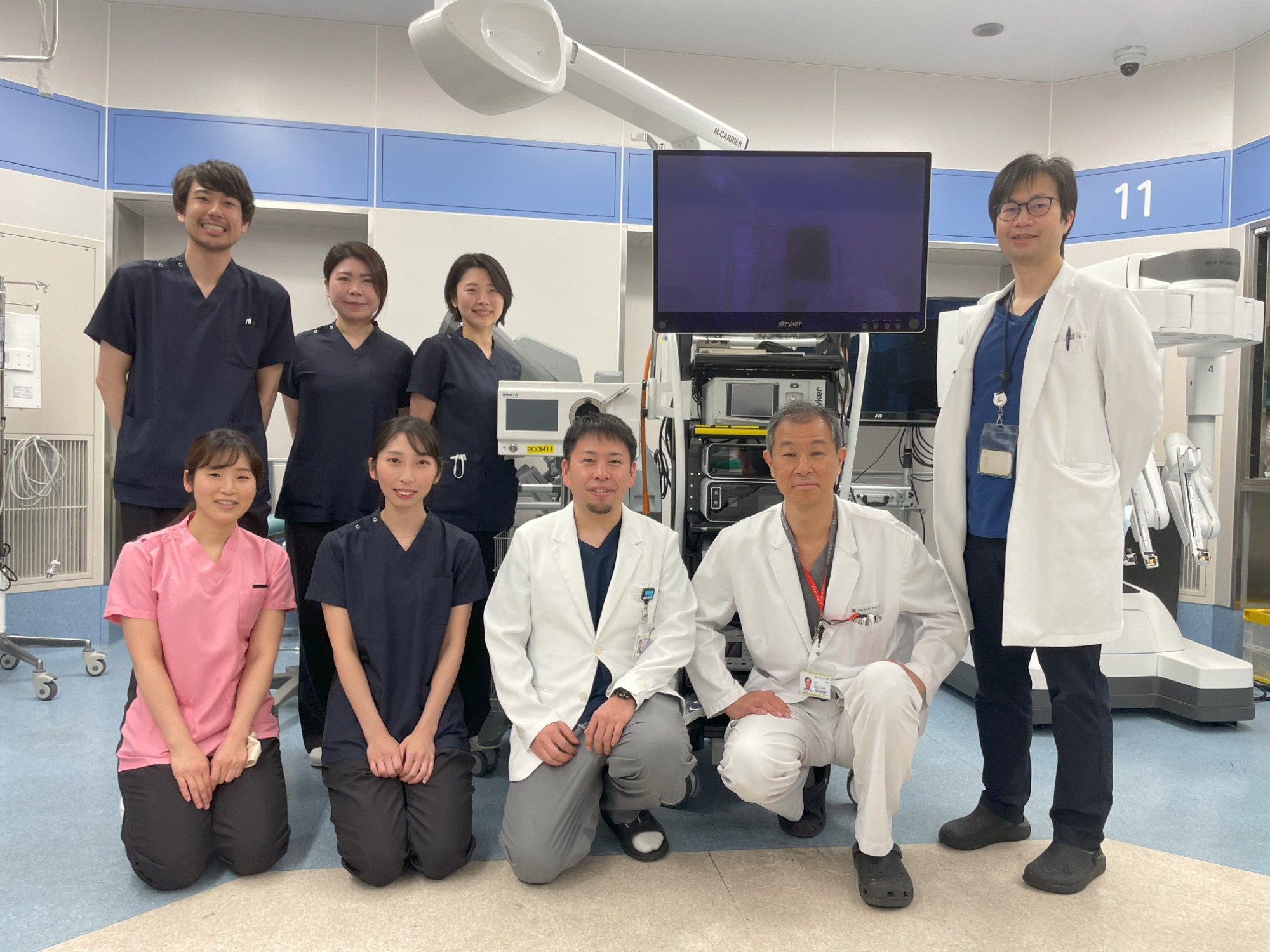
From the top left: Katsuya Tanaka, Eriko Tanaka, Haruna Godo (Nursing Department), Kozo Kataoka (Digestive Surgery) / From the bottom left: Waka Kanaba, Yurie Tsukasaki (Nursing Department), Kazuma Ito, Masataka Ikeda (Digestive Surgery)
Topic
Subcutaneous emphysema associated with laparoscopic or robotic abdominal surgery: a retrospective single-center study
Author of the paper
Kazuma Ito, Kozo Kataoka, Yuya Takenaka, Naohito Beppu, Yurie Tsukasaki, Koichi Kohno, Hiroshi Tsubamoto, Hisashi Shinohara, Seiko Hirono, Shingo Yamamoto, Hiroki Ikeuchi, Masataka Ikeda
Research Summary
Subcutaneous emphysema is a complication of laparoscopic surgery, such as laparoscopic surgery or robotic-assisted surgery. During laparoscopic surgery, the abdominal cavity is inflated with carbon dioxide (pneumoperitoneum). This can lead to accumulation of carbon dioxide gas under the skin (subcutaneous emphysema) and elevated blood carbon dioxide levels (hypercapnia). Subcutaneous emphysema and hypercapnia have been reported to cause difficulty in extubation (weaning from a ventilator) after surgery, as well as tachycardia, hypertension, arrhythmia, and other conditions.
In this study, surgeons in charge of abdominal surgery and operating room nurses jointly investigated the relationship between patient background and surgical factors and the occurrence of subcutaneous emphysema in laparoscopic surgery (laparoscopic surgery, robotic surgery) performed in our hospital's abdominal surgery departments (upper gastrointestinal surgery, lower gastrointestinal surgery, inflammatory bowel disease surgery, hepato-biliary-pancreatic surgery, obstetrics and gynecology, and urology) between April 1, 2019 and September 30, 2022, and explored the incidence of subcutaneous emphysema, the proportion of cases in which extubation was not possible, and risk factors for the occurrence of subcutaneous emphysema.
Research Background
Laparoscopic surgery is becoming more common in a variety of fields due to its minimal invasiveness compared to traditional open surgery. However, complications related to pneumoperitoneum, such as hypercapnia, subcutaneous emphysema, pneumothorax, and pneumomediastinum, have been reported in laparoscopic surgery, robotic-assisted surgery, and other laparoscopic procedures. Among these, subcutaneous emphysema is known to be the most common complication, with an incidence rate of approximately 3% according to existing reports.
However, X-rays and CT scans performed immediately after surgery revealed a very high incidence rate of approximately 24-56%. Subcutaneous emphysema during laparoscopic surgery can extend from the abdomen to the chest wall and even the neck, occasionally causing pneumothorax and difficult extubation. Previous studies have reported that risk factors for subcutaneous emphysema include high intraabdominal pressure, high carbon dioxide concentrations in exhaled breath, prolonged surgery, and a large number of ports (incisions made during laparoscopic surgery). Recent studies have also shown that robotic-assisted surgery increases the risk of developing subcutaneous emphysema compared with laparoscopic surgery. However, robotic-assisted surgery is a recently introduced procedure, and its clear causal relationship with the increased incidence of subcutaneous emphysema and its impact on the clinical course have not been fully investigated.
Research Methods and Results
We collected and analyzed information on 2,503 patients who underwent laparoscopic or robotic-assisted surgery in our hospital's abdominal surgery departments (upper gastrointestinal surgery, lower gastrointestinal surgery, inflammatory bowel disease surgery, hepato-biliary-pancreatic surgery, obstetrics and gynecology, and urology) between April 1, 2019, and September 30, 2022. The incidence of subcutaneous emphysema, the incidence of difficult extubation, and risk factors for subcutaneous emphysema were evaluated. The presence or absence of subcutaneous emphysema was confirmed either by chest and abdominal X-ray immediately after surgery or by intraoperative palpation by a nurse.
Subcutaneous emphysema was observed in 577 (23.1%) of 2,503 patients who underwent laparoscopic or robotic-assisted surgery. Subcutaneous emphysema affecting the neck was observed in approximately 5.9% of all cases, and approximately one-third of patients with subcutaneous emphysema in the neck experienced difficult extubation. Risk factors for the development of subcutaneous emphysema were identified as female gender, older age (over 80 years), low BMI (BMI 20 or less), prolonged surgery (over 360 minutes), robotic-assisted surgery, high intraabdominal pressure (intraperitoneal pressure), and end-tidal carbon dioxide concentration (the concentration of carbon dioxide at the end of exhalation).
Furthermore, these factors, except for age, were also identified as independent risk factors for severe subcutaneous emphysema (subcutaneous emphysema extending to the neck), which can cause difficult extubation. These risk factors were similar to those previously reported. Factors such as older age, low BMI, and robotic-assisted surgery have been reported to be associated with fragility of body tissues. Elderly and thin patients have less subcutaneous fat and more fragile tissues, which can lead to destruction of abdominal wall tissue during surgical procedures, making them more susceptible to developing subcutaneous emphysema.
In addition, robotic surgery uses much stronger force than human manipulation, which can destroy the abdominal wall at the port insertion site and cause subcutaneous emphysema. Given the recent increase in robotic-assisted surgery, more careful intraoperative monitoring is required.
Furthermore, the amount of carbon dioxide insufflation into the abdominal cavity is also involved in the development of subcutaneous emphysema. High abdominal pressure and end-tidal carbon dioxide concentration have also been identified as risk factors for the development of severe subcutaneous emphysema. It is necessary to control intraperitoneal pressure and carbon dioxide concentration through appropriate ventilation during surgery.
The incidence of subcutaneous emphysema in this study was higher than previously reported. This is likely due to thorough postoperative X-ray examinations and regular intraoperative palpation by nurses. Although the incidence of subcutaneous emphysema was high, the incidence of severe subcutaneous emphysema was relatively lower than in previous reports. Severe subcutaneous emphysema occurred in approximately 80% (26/33 cases) of surgeries requiring head-down positioning. The low incidence of severe subcutaneous emphysema at our hospital may be due to our efforts to release the head-down position every three hours during surgery and to have nurses palpate every hour. When subcutaneous emphysema was discovered during surgery, it was reported to the surgeon and anesthesiologist, and immediate intervention minimized the risk of subcutaneous emphysema worsening.
Although the incidence rate is quite low, severe subcutaneous emphysema, which can lead to difficult extubation, was confirmed. The identified risk factors, such as the increasing aging population and the development of robotic-assisted surgery, will be unavoidable in future medical care. This study analyzed past data from our hospital only, and furthermore, information on anesthesia management, such as the total amount of carbon dioxide used for pneumoperitoneum, ventilator settings, and fluid volume, which may affect the occurrence of subcutaneous emphysema, was lacking. Monitoring intraperitoneal pressure and end-tidal carbon dioxide concentration is essential when performing laparoscopic surgery on elderly or thin patients. Strict management is required, especially in elderly patients, to avoid difficult extubation.
Future challenges
Source of research funds etc.
None
Publication
Surg Endosc. 2024 Feb 20. doi: 10.1007/s00464-024-10701-5. Online ahead of print.