Development of an artificial ovary using decellularized human ovarian tissue
Information updated: July 31, 2023
- Seeds Information
- Researcher Information
- What do you expect from collaboration with companies?
- Contact for this research
Seeds Information
keyword
Cancer reproduction, ovarian freezing, decellularization, artificial ovary
Field
Cancer Reproduction
Overview
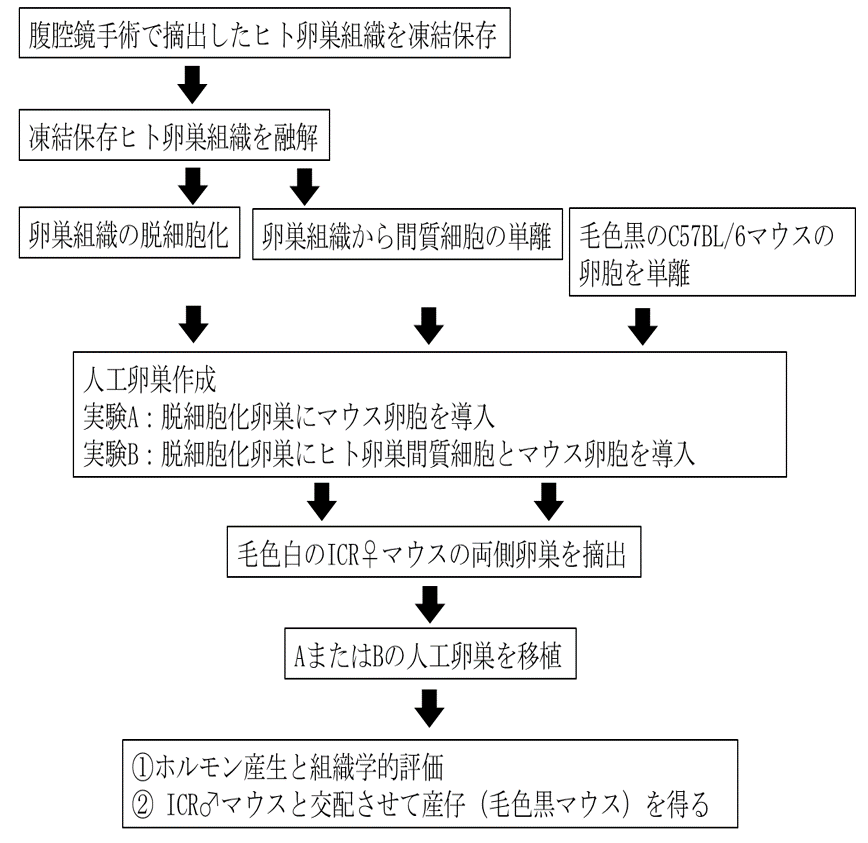
Ovarian freezing has been applied to preserve the fertility of young women with cancer, and over 180 live births have been achieved after thawing and transplantation worldwide. However, if minimal residual disease (MRD) is present in the frozen ovaries due to cancer metastasis, transplantation may lead to recurrence of the original disease. To avoid recurrence, a method has been considered in which isolated follicles are introduced into a transplantable artificial matrix to create an artificial ovary and then transplanted. Currently, artificial ovaries that mimic natural organs are being developed using artificial materials such as alginate and fibrin. Meanwhile, in recent years, it has been reported that artificial ovaries with MRD removed can be created by decellularizing human ovarian tissue. Unlike conventional gel matrices, this is a matrix derived from a living organism, so it retains factors that promote cell-cell interactions necessary for follicle development. In this study, as a model experiment, mouse follicles are introduced into decellularized human ovarian tissue and transplanted into immunodeficient mice to examine their developmental ability. The research method involves decellularizing human ovarian tissue, isolating interstitial cells from the ovarian tissue at the same time, and isolating follicles from black C57BL/6 mice. Artificial ovary group A was created by introducing black C57BL/6 mouse follicles into decellularized ovaries, while artificial ovary group B was created by introducing human ovarian stromal cells and black C57BL/6 mouse follicles into decellularized ovaries. Either artificial ovary A or artificial ovary B was implanted into white ICR female mice that had had both ovariectomized, and hormone production was confirmed and follicular development was histologically compared between the two groups. These were then mated with white ICR mice to obtain offspring (black mice).
What's new?
The artificial ovary uses decellularized human ovarian tissue instead of the conventional gel matrix.
What are its advantages over other studies?
Unlike conventional artificial gel matrices, this is a matrix of biological origin, and therefore contains factors that promote the intercellular interactions necessary for follicle development, which is thought to make it easier to produce live births.
What problem does it help solve?
Ovarian freezing is used to preserve fertility in young women with cancer, but avoiding recurrence of the original disease due to MRD remains a challenge.
By using the "artificial ovary made from decellularized human ovarian tissue" into which isolated human primordial follicles established in this study are introduced, theoretically there will be no MRD and live births will be obtained without recurrence of the primary disease due to transplantation.
Possibility of other applications and developments
―
Related Patents
―
Related papers
- Hasegawa A et al., Fertility and sterility. 2006 Oct 1;86(4):1182-92.
- SE Pors et al., Human Reproduction, 2019, 34(8), 1523–1535
- Dolmans MM et al., Reproduction. 2019 Nov;158(5):F15-F25.
- Hadrian M Kinnear, et al. Reproduction. 2020 Sep; 160: R25-R39.
- Miyazaki K et al., Biomaterials. 2014 Oct;35(31):8791-8800.
Researcher Information
| full name | Yutaka Wakimoto |
|---|---|
| Affiliation | School of Medicine Department of Obstetrics and Gynecology |
| Specialization | Cancer Reproduction |
| Collaborative Researcher | Chen Yuekhun, Nakagawa Kohei, Hasegawa Akiko, Shibahara Hiroaki |
| Related links | Course introduction website |
What do you expect from collaboration with companies?
By collaborating with companies, we aim to develop an artificial ovary that is safer and makes it easier to obtain live births while resolving the following issues:
- Since human ovarian tissue containing leukemia cells is difficult to obtain, it will be necessary to create leukemia model mice transplanted with human ovarian tissue and examine whether decellularization can remove microscopic residual cancer lesions.
- Since decellularized tissue does not contain theca cells, androgens, the precursors of female hormones, are not produced, which is thought to impair follicle formation. It is possible to apply the fact that when ovarian stromal cells are cultured together with ovarian granulosa cells, some of them differentiate into theca cells.
- Native collagen, the main component of decellularized tissue, has low immunogenicity even though it is a xenogeneic tissue, and there is almost no foreign body (rejection) reaction when transplanted, so we will investigate Department of Immunology involvement during transplantation.
- We would like to conduct collaborative research to develop a device that can efficiently introduce eggs into decellularized ovarian tissue.
Contact for this research
兵庫医科大学 大学事務部 研究推進課
E-mail: chizai@hyo-med.ac.jp
Tel: 0798-45-6488
 Research Seeds Collection
Research Seeds Collection